Skin Condition Disease
- Compromised Skin Flap/ Graft
- Necrotising Fasciitis (Flesh Eating Disease)
- Diabetic Foot (Non Healing Wounds)
- Thermal/ Extensive Burns
- Cosmetic Surgery Aftercare
HBOT For Compromised Skin Flap/ Graft
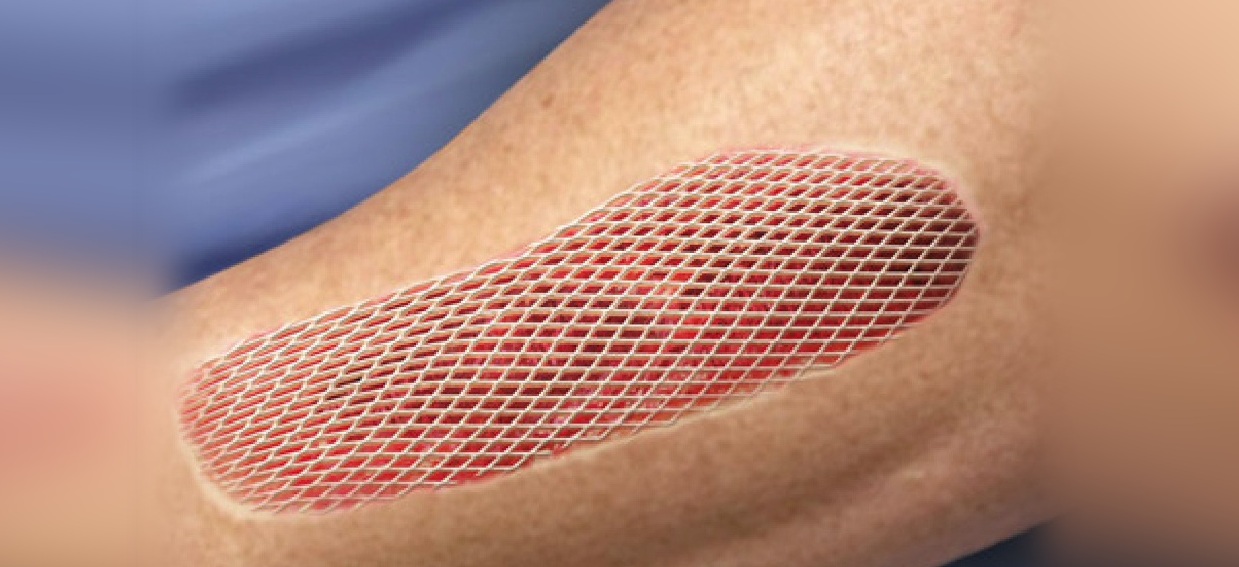
A flap is a section of healthy skin that is partially detached and moved to cover a nearby wound. The flap has its own blood supply. This allows the old blood supply to remain intact while a new blood supply develops. A graft is a piece of healthy skin that is removed from one part of the body and used to cover a wound elsewhere. Unlike a skin flap, a graft does not have its own blood supply. A skin flap may contain skin and fat, or skin, fat, and muscle. Poor flap design is one of the most common causes of flap failure. Inadequate flap size, violation of the blood supply to the flap, or design of the flap in radiated or traumatized tissue often causes early problems in the surgical procedure. A freshly applied split-thickness graft receives no oxygen until tiny blood vessels called capillaries can penetrate it. Such capillary ingrowth normally takes place over a two to three day period. If this does not happen, it’s unlikely that the graft will survive. HBOT improves the chances that a graft will take, both by supplying oxygen and by encouraging quick capillary growth. Providing hyper oxygenation increases the oxygen tension in the graft bed and wound margins up to 1500 percent. It also causes a marked increase in the amount of oxygen that reaches the graft through the compromised blood vessels. The volume of tissue that derives sufficient oxygen from a single damaged blood vessel increases 16 fold, and marked tissue salvage results. Lack of oxygen tends to be less of a problem with full-thickness and pedicle grafts since these grafts have their own supply of capillaries. Even so, it still takes time for good blood flow to become established through these types of grafts, Therefore full-thickness and pedicle grafts also respond to HBOT. In many instances HBOT is used only after a skin graft starts to fail.
Benefits of HBOT :Skin grafts immediately become ischemic or hypoxic on harvest. The recipient bed must be healthy enough to accept and nourish a graft. The goal is to identify wounds that have failed usual therapy, and flap coverage that can respond locally to HBOT. In some cases, HBOT will be enough to make skin grafting unnecessary or reduce re-grafting and repeat flap procedures. Indications for adjunctive HBOT for flaps and grafts include preparing a granulating base in selected patients with compromised wounds (diabetic ulcer, venous stasis ulcer, arterial insufficiency ulcer) or flaps, and patients at high risk due to previous failures. Oxygen availability is critical to skin grafting success. HBOT increases tissue oxygen levels in hypoxic and ischemic wounds. HBOT stimulates formation of blood vessels and granulation tissue, and prepares the recipient bed for grafts or flaps. It also improves wound healing, namely, improved fibroblast and collagen synthesis. While HBOT can help save failing grafts it can be even more effective when used before surgery to keep grafts from failing in the first place. HBOT also offers strategies for reducing edema. The edema reduction effect, induced by the relative spasm of a precapillary arteriolar sphincter helps to limit the swelling of the graft or flap. The high oxygen tension achievable with HBOT induces neovascularization. Among other things, oxygen dissolved in plasma is readily available to tissues and organs thus limiting damage from reperfusion injury. HBOT’s effectiveness in aiding skin graft survival is supported by research. The effectiveness of HBOT is shown in grafting and in reimplantation of limbs, with a salvage rate of 75% for the HBOT group compared to 46% for the controls, with 100% HBOT salvage when the patient is treated within 72 hours post-operatively.